Fundus fluorescein angiography (FFA) and optical coherence tomography-angiography (OCT-A) demonstrate similar consistencies for diagnosing diabetic retinopathy (DR), but post-panretinal photocoagulation lesions may be best evaluated with OCT-A assessment, according to findings published in the Journal Français d’Ophtalmologie.
The study included patients with diabetes who received a DR diagnosis with both FFA and OCT-A evaluations (n=96; eyes, 185; 57 men; mean age, 58.27 years). Participants underwent retinal nerve fiber layer (RNFL) thickness, macular superficial vascular complex (SVC) and deep vascular complex (DVC) blood flow density, and 300 µm area surrounding the foveal avascular zone (FD300) blood flow density measurements.
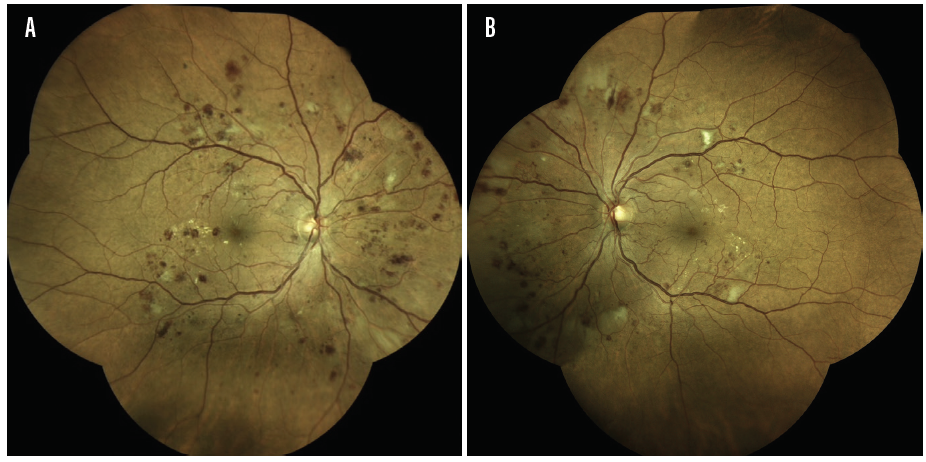
The FFA analysis revealed 158 eyes met the criteria for DR and 27 did not. The OCT-A assessment confirmed a positive diagnosis in 142 of those cases while rendering a negative diagnosis for 16 eyes. A total of 19 eyes receiving a negative DR diagnosis through FFA were confirmed by OCT-A and 8 eyes with a negative diagnosis via FFA received a positive DR diagnosis with OCT-A (κ, 0.537; P =0.000).
Both imaging methods demonstrated consistency for detecting retinal microaneurysms (κ, 0.643), macular edema (κ, 0.616), retinal neovascularization (κ, 0.809), non-perfusion area (κ, 0.832), and structural changes in the macular ring (κ, 0.423; all P =.000), the report shows.
A subset of 137 eyes (n=69) underwent post-panretinal photocoagulation. The OCT-A analysis detected significant changes at 1 year compared with baseline with respect to DVC blood flow density (t, 13.516; P =0.000), FD300 blood flow density, SVC flow density (t, 9.675; P =0.000), and RNFL thicknesses in the inferior nasal (t, 7.365; P =0.000), superior temporal (t, 6.802; P =0.000), temporal inferior (t, 6.588; P =0.000), and superior nasal (t, 5.083; P =0.000) regions.
The study authors stress the need for consistent diagnostic methods. “Most diabetic patients have no obvious symptoms in the [non proliferative diabetic retinopathy] stage,” according to the researchers. “When they visit doctors with evident visual dysfunction, however, most of the retinal lesions have progressed to the middle and late stages, missing the optimal treatment window. Therefore, the early detection and timely intervention of DR are of great clinical significance.”
Study limitations include a small sample size, single center design, and failure to stratify patients according to lesion severity.
Huang Y, Kong X, Zhou L, Shen P, Su P, Su H. Values of optical coherence tomography angiography for diagnosing diabetic retinopathy and evaluating treatment outcomes. J Fr Ophtalmol. Published online December 2, 2022. doi:10.1016/j.jfo.2022.05.030